Extreme fatigue 6 months after gastric sleeve surgery can be a concerning symptom that may require attention. After gastric sleeve surgery, your doctor will provide you with specific dietary guidelines to follow during the different phases of your recovery. While I can offer some general information, it’s important to consult with your healthcare provider or a registered dietitian who specializes in bariatric surgery for personalized advice.
Get a $1000 Off on Gastric Sleeve in Miami
Recognizing When Extreme Fatigue Requires Medical Attention
Extreme fatigue can be a symptom of various underlying medical conditions. While occasional tiredness is normal, persistent and severe fatigue that interferes with your daily activities and doesn’t improve with rest may warrant medical attention. Here are some signs that indicate you should seek medical advice:
- Duration and severity: If your extreme fatigue persists for an extended period, such as weeks or months, or if it becomes progressively worse, it’s important to consult a healthcare professional. Extreme fatigue that significantly impacts your ability to function and doesn’t improve with rest should not be ignored.
- Other accompanying symptoms: Pay attention to other symptoms that may accompany your extreme fatigue. Examples include unexplained weight loss, persistent headaches, difficulty concentrating, frequent infections, mood changes, muscle weakness, or any other unusual or concerning symptoms.
- Impact on daily life: If your fatigue prevents you from engaging in your usual activities, such as work, socializing, or hobbies, it’s essential to seek medical advice. Fatigue that limits your ability to perform basic tasks or interferes with your quality of life requires attention.
- Chronic conditions: If you have pre-existing medical conditions such as diabetes, thyroid disorders, autoimmune diseases, or other chronic illnesses, extreme fatigue could be a sign of a worsening or new problem. In such cases, it’s important to consult your healthcare provider to evaluate the potential underlying causes.
- Changes after a specific event or treatment: If your extreme fatigue started or worsened after a particular event, such as surgery, medication changes, or any other medical intervention, it’s crucial to inform your healthcare provider. They can assess whether the fatigue is related to the event or treatment and provide appropriate guidance.
Remember, extreme fatigue can have various causes, including physical, mental, and emotional factors. Consulting a healthcare professional is essential to determine the underlying cause and develop an appropriate treatment plan. They can conduct a thorough evaluation, consider your medical history, order necessary tests, and provide personalized advice based on your specific situation.

Identifying and Addressing Persistent Fatigue
Persistent fatigue can have multiple causes, and it’s important to work with a healthcare professional to identify and address the underlying factors. Here are some steps you can take:
- Consult a healthcare provider: If you’re experiencing persistent fatigue, schedule an appointment with a healthcare professional. They can evaluate your symptoms, review your medical history, and conduct necessary tests to help determine the underlying cause.
- Rule out medical conditions: Your healthcare provider may perform blood tests to check for potential underlying medical conditions that could contribute to fatigue, such as anemia, thyroid disorders, vitamin deficiencies, or chronic infections. Treating any identified conditions can help alleviate fatigue.
- Review medications and supplements: Certain medications or supplements can cause fatigue as a side effect. Discuss with your healthcare provider whether any of your current medications could be contributing to your fatigue. They may suggest adjustments or alternatives if appropriate.
- Assess sleep quality: Poor sleep quality or sleep disorders, such as sleep apnea, can lead to persistent fatigue. Discuss your sleep patterns with your healthcare provider, who may refer you to a sleep specialist for evaluation and appropriate treatment.
- Evaluate lifestyle factors: Lifestyle choices can influence energy levels. Assess your daily routine, including diet, exercise, and stress management. Aim for a balanced diet, engage in regular physical activity (if cleared by your healthcare provider), and explore stress-reduction techniques, such as mindfulness or relaxation exercises.
- Manage stress: Chronic stress can contribute to fatigue. Identify stressors in your life and seek healthy coping mechanisms, such as exercise, hobbies, social support, or counseling. If necessary, consider speaking with a mental health professional to address any underlying emotional factors.
- Pace yourself and prioritize rest: Pushing yourself too hard or overcommitting can exacerbate fatigue. Learn to pace yourself and prioritize rest. Allow yourself breaks throughout the day, practice good sleep hygiene, and ensure you’re getting adequate restorative sleep.
- Consider nutritional support: If your healthcare provider identifies any nutritional deficiencies, they may recommend dietary changes or supplements. Follow their guidance to address any specific nutrient imbalances that could be contributing to fatigue.
The Importance of Open Communication with Your Healthcare Provider
Open communication with your healthcare provider is crucial for ensuring quality care and maintaining your overall well-being. Here are several reasons why it’s important to have open and transparent communication with your healthcare provider:
| Importance of Open Communication with Your Healthcare Provider |
|---|
| 1. Accurate diagnosis and treatment |
| 2. Shared decision-making |
| 3. Understanding risks and benefits |
| 4. Monitoring progress and adjusting treatment |
| 5. Preventing medical errors |
| 6. Addressing emotional and mental health needs |
| 7. Building trust and rapport |
Nutritional Deficiencies and Imbalances
Nutritional deficiencies and imbalances occur when there is an inadequate intake or absorption of essential nutrients, or when there is an excessive intake of certain nutrients. These imbalances can have significant health implications. Here are some common nutritional deficiencies and imbalances:
- Iron deficiency: Iron is essential for the production of red blood cells and oxygen transport. Iron deficiency can lead to anemia, resulting in fatigue, weakness, and impaired cognitive function.
- Vitamin D deficiency: Vitamin D is crucial for bone health, immune function, and overall well-being. Inadequate sun exposure and limited dietary sources can lead to vitamin D deficiency, which may contribute to weakened bones, muscle pain, and increased risk of infections.
- Vitamin B12 deficiency: Vitamin B12 is necessary for nerve function and the production of red blood cells. Deficiency can result in anemia, neurological problems, fatigue, and cognitive difficulties.
- Calcium deficiency: Calcium is essential for strong bones and teeth, muscle function, and nerve transmission. Inadequate calcium intake can increase the risk of osteoporosis and fractures.
- Iodine deficiency: Iodine is required for thyroid hormone production, which regulates metabolism. Insufficient iodine intake can lead to thyroid disorders, including goiter and hypothyroidism.
- Omega-3 fatty acid imbalance: Omega-3 fatty acids are important for brain function, heart health, and reducing inflammation. Imbalances between omega-3 and omega-6 fatty acids, often due to a high intake of processed foods, can contribute to chronic inflammation and increased risk of cardiovascular disease.
- Sodium/potassium imbalance: An imbalance between sodium and potassium levels can affect blood pressure regulation and increase the risk of hypertension. Excessive sodium intake and inadequate potassium intake are common in Western diets.
- Excessive sugar intake: Consuming excessive amounts of added sugars can lead to weight gain, increased risk of type 2 diabetes, dental problems, and cardiovascular issues.
It’s important to maintain a balanced and varied diet to prevent nutritional deficiencies and imbalances. If you suspect you have a deficiency or imbalance, consult with a healthcare provider or registered dietitian who can evaluate your specific needs and provide guidance on appropriate dietary changes or supplementation.
Inadequate Caloric Intake and Energy Levels
Inadequate caloric intake can have a significant impact on energy levels. When your body does not receive enough calories to meet its energy needs, it can lead to fatigue and decreased overall energy levels. Here are a few ways inadequate caloric intake can affect your energy levels:
- Insufficient fuel for bodily functions: Calories provide the energy necessary for your body’s basic functions, such as breathing, digestion, and circulation. When you don’t consume enough calories, your body may prioritize essential functions, resulting in decreased energy for other activities.
- Muscle weakness and fatigue: Inadequate caloric intake can lead to muscle weakness and fatigue. Muscles require energy in the form of calories to contract and perform various physical activities. Without enough calories, your muscles may not function optimally, resulting in reduced energy levels and decreased physical performance.
- Mental fatigue and difficulty concentrating: The brain relies on glucose, which comes from dietary carbohydrates, as its primary source of fuel. Inadequate caloric intake, particularly from carbohydrates, can result in mental fatigue, difficulty concentrating, and reduced cognitive function.
- Nutrient deficiencies: Inadequate caloric intake may also contribute to nutrient deficiencies. When you consume fewer calories than your body needs, it can be challenging to obtain sufficient amounts of essential vitamins, minerals, and other nutrients. These deficiencies can further impact energy levels and overall well-being.

To address inadequate caloric intake and boost energy levels, it’s important to:
- Ensure you’re consuming a balanced diet that includes a variety of nutrient-dense foods.
- Pay attention to portion sizes and eat enough calories to meet your body’s energy needs.
- Include a mix of carbohydrates, proteins, and healthy fats in your meals to provide sustained energy.
- Listen to your body’s hunger and fullness cues and eat when you’re hungry.
- Consider working with a registered dietitian who can help assess your caloric needs and create a personalized meal plan.
It’s worth noting that if you’re experiencing prolonged fatigue or have concerns about your energy levels, it’s essential to consult with a healthcare professional. They can evaluate your specific situation, conduct any necessary tests, and provide appropriate recommendations to address your concerns.
Hormonal Changes and Metabolic Adaptations
Hormonal changes and metabolic adaptations can have a significant impact on the body’s energy levels and overall functioning. Here are a few examples of how hormonal changes and metabolic adaptations can affect energy levels:
| Hormonal Changes and Metabolic Adaptations Impacting Energy Levels |
|---|
| Thyroid Hormones |
| Insulin and Blood Sugar Regulation |
| Leptin and Ghrelin Regulation |
| Metabolic Adaptations |
| Stress Hormones |
Adopting a Balanced and Nutrient-Rich Diet
Adopting a balanced and nutrient-rich diet is crucial for maintaining optimal health and energy levels. Here are some key principles to keep in mind when striving for a balanced and nutrient-rich diet:
- Include a variety of fruits and vegetables: Aim to incorporate a wide range of fruits and vegetables into your meals. They are rich in vitamins, minerals, antioxidants, and dietary fiber, which support overall health and provide essential nutrients.
- Prioritize whole grains: Choose whole grains over refined grains. Whole grains such as quinoa, brown rice, whole wheat bread, and oats provide more fiber, vitamins, and minerals than their refined counterparts, promoting sustained energy and better overall nutrition.
- Opt for lean proteins: Include lean sources of protein in your diet, such as poultry, fish, tofu, legumes, and low-fat dairy products. Protein is essential for muscle function, energy production, and overall body repair and maintenance.
- Don’t forget healthy fats: Incorporate sources of healthy fats, such as avocados, nuts, seeds, and olive oil, into your diet. Healthy fats provide energy, support brain function, and aid in the absorption of fat-soluble vitamins.
- Limit added sugars and processed foods: Minimize the intake of added sugars, sugary beverages, and highly processed foods. These can lead to energy crashes, weight gain, and an increased risk of chronic diseases.
- Stay hydrated: Drink an adequate amount of water throughout the day to maintain hydration. Dehydration can contribute to fatigue and decreased energy levels.
- Practice portion control: Pay attention to portion sizes and avoid overeating. Even nutrient-rich foods should be consumed in moderation to maintain a healthy balance of calories.
Remember, adopting a balanced and nutrient-rich diet is a long-term commitment to your health. It’s about making consistent, positive changes to your eating habits rather than following strict diets.
The Recovery Process After Gastric Sleeve Surgery
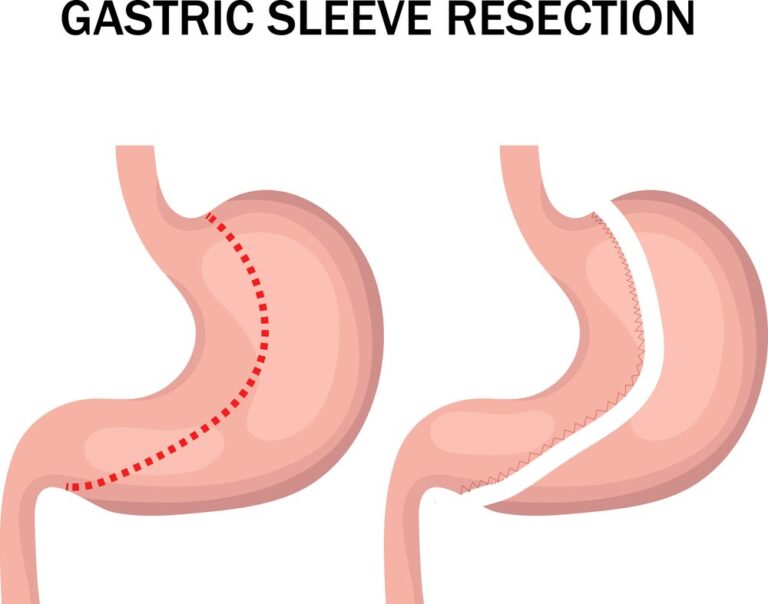
The recovery process after gastric sleeve surgery, also known as sleeve gastrectomy, involves several stages. While individual experiences may vary, here are some general aspects to consider:
- Hospital stay: Following the surgery, you will typically stay in the hospital for one to two days. During this time, medical professionals will monitor your condition, manage pain and discomfort, and provide instructions for your post-operative care.
- Post-operative diet stages: After gastric sleeve surgery, your diet will progress through several stages:
- Clear liquids: In the initial days after surgery, you’ll start with a clear liquid diet, including water, broth, sugar-free gelatin, and clear protein drinks.
- Full liquids: You’ll then progress to full liquids, which can include protein shakes, low-fat milk, and strained soups.
- Pureed foods: After about two to four weeks, you’ll transition to pureed or mashed foods. These should be smooth in texture and easy to digest.
- Soft foods: Around four to six weeks after surgery, you can start incorporating soft, well-cooked foods into your diet.
- Solid foods: Eventually, you’ll reintroduce solid foods. However, it’s important to follow the guidelines provided by your healthcare team and focus on portion control, balanced nutrition, and adopting healthy eating habits.
- Physical activity: Initially, you’ll need to rest and avoid strenuous activities. As you progress in your recovery, your healthcare provider will advise you on gradually increasing physical activity. Regular exercise is important for maintaining weight loss, improving fitness, and promoting overall health.
- Follow-up appointments: You will have regular follow-up appointments with your healthcare team to monitor your progress, address any concerns, and make adjustments to your diet or medication, if necessary.
- Lifestyle changes and support: Gastric sleeve surgery is a tool to help facilitate weight loss, but long-term success relies on adopting healthy lifestyle habits. This includes making nutritious food choices, engaging in regular physical activity, managing stress, and seeking support from healthcare professionals, support groups, or counseling if needed.
References:
- Cleveland Clinic. (2022). After Weight Loss Surgery: Bariatric Surgery Recovery Timeline. Retrieved June 6, 2022
- Obesity Action Coalition. (2022). Life After Bariatric Surgery. Retrieved Jan 6, 2022