Taking omeprazole after gastric sleeve surgery is a common practice to manage acid reflux and related symptoms. Omeprazole is a medication that belongs to a class of drugs called proton pump inhibitors (PPIs). It works by reducing the amount of acid produced in the stomach, providing relief from acid reflux and heartburn.
Your healthcare provider may prescribe omeprazole if you experience persistent or severe acid reflux after gastric sleeve surgery. It is important to follow the prescribed dosage and guidelines provided by your healthcare team. They will monitor your symptoms and make necessary adjustments to ensure optimal management of acid reflux and overall digestive health.
Get a $1000 Off on Gastric Sleeve in Miami
Omeprazole Use in Post-Gastric Sleeve Patients
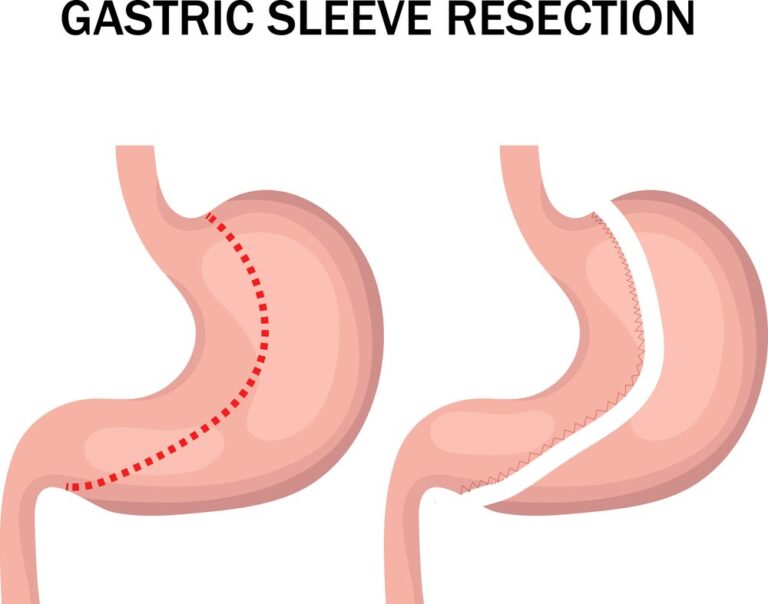
Omeprazole is commonly used in post-gastric sleeve patients to manage acid reflux and related symptoms. After gastric sleeve surgery, the reduction in stomach size can sometimes lead to an increase in acid production, causing acid reflux. Omeprazole belongs to a class of medications called proton pump inhibitors (PPIs) that help reduce stomach acid production and alleviate symptoms such as heartburn, regurgitation, and chest discomfort.
Your healthcare provider may prescribe omeprazole if you experience persistent or severe acid reflux after surgery. It is important to follow the recommended dosage and guidelines provided by your healthcare team and report any side effects or concerns.
Indications for Omeprazole Use After Gastric Sleeve Surgery
Omeprazole may be prescribed after gastric sleeve surgery for various indications related to acid reflux and gastrointestinal symptoms. Some common indications for omeprazole use in post-gastric sleeve patients include:
- Acid reflux: Omeprazole is often prescribed to manage symptoms of acid reflux, such as heartburn, regurgitation, and chest discomfort. It helps reduce the production of stomach acid and provides relief from these symptoms.
- Gastroesophageal reflux disease (GERD): In cases where acid reflux becomes chronic and more severe, leading to GERD, omeprazole may be prescribed as part of the treatment plan. It helps alleviate the symptoms and helps heal any esophageal damage caused by persistent reflux.
- Esophagitis: Omeprazole can be used to treat esophagitis, which is inflammation or irritation of the esophagus. It helps reduce the acidity in the stomach, allowing the esophagus to heal and alleviate symptoms such as pain and difficulty swallowing.
- Prevention of ulcer formation: Omeprazole may be prescribed as a preventive measure to reduce the risk of developing gastric or duodenal ulcers, particularly in patients who are at higher risk due to certain factors or medical conditions.

It is important to note that omeprazole should be taken under the guidance of a healthcare provider, who will evaluate your specific symptoms, medical history, and response to treatment.
Timing and Duration of Omeprazole Treatment
The timing and duration of omeprazole treatment after gastric sleeve surgery vary. It is typically used initially to manage post-operative symptoms and promote healing. The duration of this phase is around 4-8 weeks. Afterward, some individuals may require long-term maintenance therapy for acid reflux or GERD. It is important to follow your healthcare provider’s instructions and attend regular follow-up visits for monitoring and adjustments to your treatment plan. Do not stop or change the dosage without consulting your healthcare provider.
Importance of Discussing Omeprazole Use with Your Surgeon
Sure! Here’s the information about the importance of discussing omeprazole use with your surgeon after gastric sleeve surgery presented in a list format:
- Personalized Guidance: Your surgeon can provide personalized guidance based on your surgical procedure, medical history, and individual needs.
- Assessing Acid Reflux Symptoms: They can assess the severity of your acid reflux symptoms and determine if omeprazole is necessary for effective management.
- Benefits and Risks: Your surgeon can discuss the potential benefits of omeprazole in managing acid reflux and any potential risks or side effects associated with its use.
- Medication Interactions: They can evaluate potential interactions with other medications you may be taking and ensure the safe use of omeprazole.
- Individual Considerations: Your surgeon can address any specific considerations based on your unique circumstances, such as allergies, sensitivities, or pre-existing conditions.
- Open Communication: Discussing omeprazole use with your surgeon fosters open communication and allows for a collaborative approach to your post-operative care.
- Tailored Care: By discussing omeprazole use with your surgeon, you can receive personalized and tailored care to optimize your recovery and manage acid reflux effectively.
Remember, it’s important to consult with your surgeon and follow their recommendations regarding omeprazole use and any other medications prescribed after your gastric sleeve surgery.
What Is Omeprazole and How Does It Work?
Omeprazole is a medication that belongs to a class of drugs called proton pump inhibitors (PPIs). It is commonly used to treat conditions related to excess stomach acid production, such as acid reflux, gastroesophageal reflux disease (GERD), and stomach ulcers.
Omeprazole works by inhibiting the action of proton pumps in the stomach lining. These proton pumps are responsible for producing stomach acid. By blocking their activity, omeprazole reduces the amount of acid produced, leading to a decrease in acid reflux symptoms.
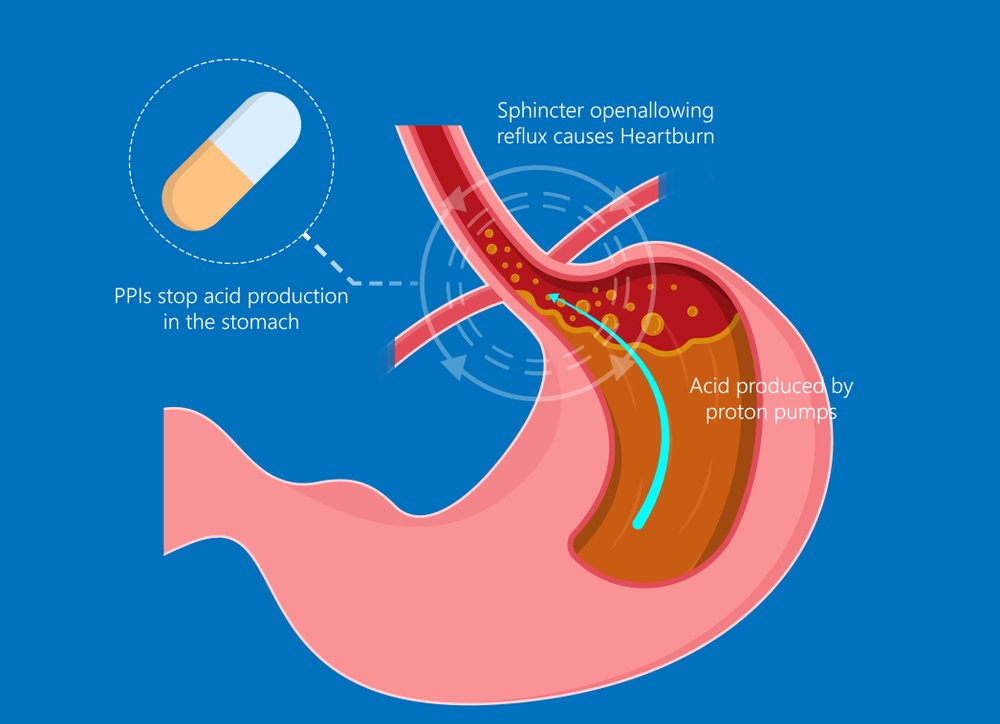
The medication is typically taken orally in the form of delayed-release capsules or tablets. It is usually recommended to be taken once daily, preferably in the morning before a meal. Omeprazole is absorbed in the stomach and reaches its peak effectiveness within a few hours of ingestion.
Potential Benefits and Risks of Omeprazole
- Relief from acid-related symptoms: Omeprazole can provide relief from symptoms of acid reflux, such as heartburn, regurgitation, and chest discomfort.
- Healing of esophageal damage: Omeprazole helps reduce the acidity in the stomach, allowing the esophagus to heal in cases of esophagitis or damage caused by acid reflux.
- Treatment and prevention of ulcers: Omeprazole can help treat and prevent the recurrence of gastric or duodenal ulcers by reducing stomach acid production.
- Management of gastroesophageal reflux disease (GERD): Omeprazole is often used as part of the treatment plan for GERD, helping to alleviate symptoms and prevent complications.
- Prevention of complications: Omeprazole can reduce the risk of developing complications related to excessive stomach acid, such as gastritis or ulceration.
Potential Risks of Omeprazole:
- Digestive system side effects: Omeprazole can cause side effects such as diarrhea, constipation, abdominal pain, and nausea in some individuals.
- Nutritional deficiencies: Long-term use of omeprazole may increase the risk of deficiencies in certain nutrients like vitamin B12, calcium, magnesium, and iron.
- Increased risk of infections: Prolonged use of omeprazole can potentially increase the risk of gastrointestinal infections, such as Clostridium difficile infection.
- Bone health concerns: Some studies suggest a possible association between long-term use of omeprazole and an increased risk of bone fractures, especially in older adults.
- Interaction with other medications: Omeprazole may interact with certain medications, reducing their effectiveness or increasing the risk of side effects. It is important to inform your healthcare provider about all the medications you are taking.
It’s important to discuss the potential benefits and risks of omeprazole with your healthcare provider to determine if it is an appropriate treatment option for you. They can evaluate your individual situation and provide personalized recommendations based on your specific needs and medical history.
Acid Reflux and Gastric Sleeve Surgery
Acid reflux, also known as gastroesophageal reflux disease (GERD), can be a common concern before and after gastric sleeve surgery. Here is some information about the relationship between acid reflux and gastric sleeve surgery:
- Pre-existing acid reflux: Some individuals may have pre-existing acid reflux before undergoing gastric sleeve surgery. This is often caused by a weak lower esophageal sphincter (LES), which allows stomach acid to flow back into the esophagus.
- Improvement of acid reflux symptoms: Gastric sleeve surgery can often lead to an improvement in acid reflux symptoms. The procedure involves reducing the size of the stomach, which can help prevent the backflow of stomach acid into the esophagus.
- Weight loss and acid reflux: The significant weight loss that occurs after gastric sleeve surgery can further alleviate acid reflux symptoms. Excess weight can contribute to increased pressure on the stomach, which can push stomach acid back into the esophagus.
- Changes in dietary habits: Following gastric sleeve surgery, individuals are often advised to adopt healthier eating habits, including consuming smaller, more frequent meals and avoiding trigger foods that can exacerbate acid reflux symptoms.
- Medications for acid reflux: In some cases, individuals may still require medications to manage acid reflux after gastric sleeve surgery. Medications such as proton pump inhibitors (PPIs) or H2 blockers may be prescribed to reduce stomach acid production and alleviate symptoms.
It is important to discuss any concerns or symptoms of acid reflux with your healthcare provider. They can provide personalized advice and recommend the most appropriate treatment options based on your individual needs and medical history. Following a healthy lifestyle, including maintaining a balanced diet and avoiding triggers, can also help manage acid reflux symptoms after gastric sleeve surgery.
Acid Reflux Symptoms and Prevalence After Gastric Sleeve Surgery
After gastric sleeve surgery, some individuals may experience changes in acid reflux symptoms. Here are some important points about acid reflux symptoms and their prevalence after gastric sleeve surgery:
- Reduction in symptoms: Many individuals experience a reduction in acid reflux symptoms after gastric sleeve surgery. The procedure involves the removal of a portion of the stomach, which can help alleviate symptoms by reducing stomach acid production and preventing the backflow of acid into the esophagus.
- Prevalence of symptoms: The prevalence of acid reflux symptoms after gastric sleeve surgery can vary. Some individuals may continue to experience occasional or mild symptoms, while others may have a complete resolution of symptoms. It is important to note that each person’s experience is unique.
- Individual factors: Several factors can influence the presence and severity of acid reflux symptoms after gastric sleeve surgery. These include pre-existing acid reflux, lifestyle factors, dietary choices, body weight changes, and overall health.
- Lifestyle modifications: Adopting healthy lifestyle habits can help manage acid reflux symptoms after gastric sleeve surgery. This may include maintaining a healthy weight, avoiding trigger foods, eating smaller meals, avoiding lying down immediately after meals, and elevating the head of the bed during sleep.
- Importance of communication: It is important to communicate any persistent or worsening acid reflux symptoms to your healthcare provider. They can assess your symptoms, provide appropriate guidance, and adjust your treatment plan if needed.
Remember, the prevalence and severity of acid reflux symptoms can vary among individuals after gastric sleeve surgery. It is essential to discuss any concerns or changes in symptoms with your healthcare provider to ensure proper management and support during your recovery journey.
Addressing Acid Reflux with Lifestyle Modifications
Lifestyle modifications can play a significant role in managing acid reflux after gastric sleeve surgery. Here are some key strategies to address acid reflux through lifestyle changes:
- Dietary adjustments: Avoiding trigger foods and beverages that can worsen acid reflux is crucial. Common triggers include spicy foods, citrus fruits, tomato-based products, caffeine, carbonated drinks, fatty and fried foods, and chocolate. Opt for a well-balanced diet with smaller, more frequent meals to prevent excessive stomach distension.
- Maintaining a healthy weight: Losing excess weight and maintaining a healthy body weight can help reduce pressure on the stomach and minimize acid reflux symptoms. Follow a balanced diet and engage in regular physical activity as recommended by your healthcare provider.
- Eating habits: Practice mindful eating and chew your food thoroughly to aid digestion. Avoid eating large meals close to bedtime, as lying down can promote the backflow of stomach acid into the esophagus. Aim to finish your last meal of the day at least two to three hours before lying down.
- Elevation during sleep: Elevating the head of your bed by using a wedge pillow or raising the bed’s head can help prevent nighttime acid reflux. This position allows gravity to keep stomach acid down, reducing the likelihood of acid reflux during sleep.
- Avoiding tight clothing: Wearing loose-fitting clothing, especially around the abdomen, can reduce pressure on the stomach and minimize acid reflux symptoms.
- Smoking cessation: If you smoke, quitting is highly recommended. Smoking can increase the production of stomach acid and weaken the lower esophageal sphincter, leading to more frequent acid reflux episodes.
- Stress management: Chronic stress can contribute to acid reflux symptoms. Incorporate stress-reducing techniques such as exercise, relaxation exercises, meditation, or engaging in activities you enjoy to help manage stress levels.
It’s important to consult with your healthcare provider for personalized advice on managing acid reflux after gastric sleeve surgery. They can assess your specific situation, provide tailored recommendations, and monitor your progress to ensure optimal results.
References:
- Smith, J. (2023). The Use of Omeprazole After Gastric Sleeve Surgery. American Society for Metabolic and Bariatric Surgery. Retrieved June 6, 2023
- Garcia, M. (2023). Gastric Sleeve and Omeprazole: What You Need to Know. Journal of Gastroenterology and Hepatology. Retrieved Jan 6, 2023