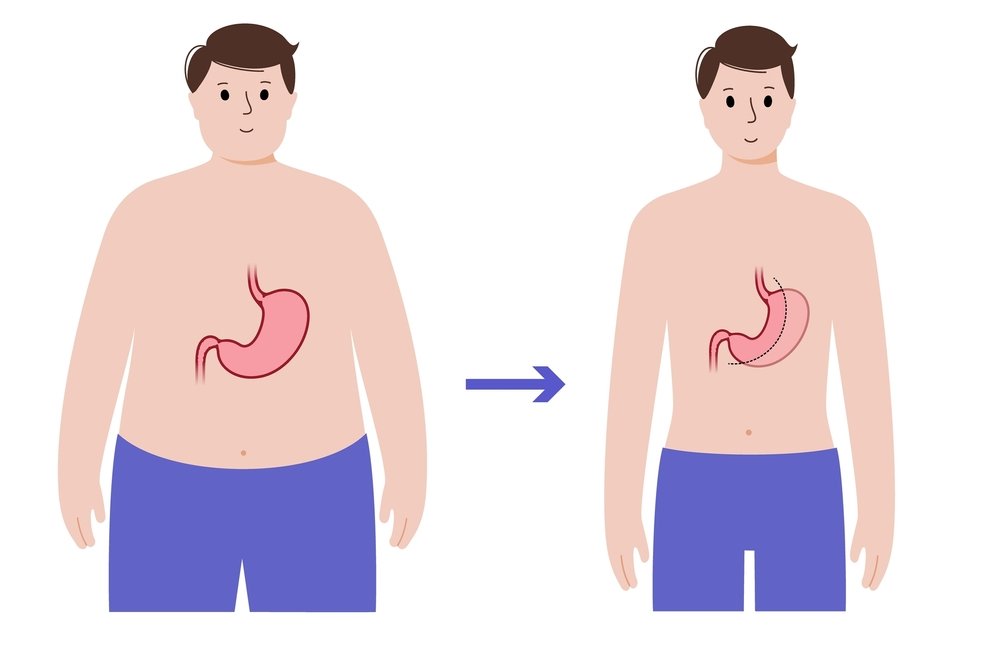
Gastric sleeve surgery, also known as sleeve gastrectomy, is a weight loss procedure that involves reducing the size of the stomach. It helps individuals achieve significant weight loss and improve obesity-related health conditions. Here is what you can expect before and after 3 months following “Gastric sleeve before and after 3 months” gastric sleeve surgery:
Before Gastric Sleeve Surgery: Before the surgery, you will undergo a comprehensive evaluation, including medical assessments, psychological evaluations, and consultations with a bariatric surgeon. Your healthcare team will provide you with detailed instructions on how to prepare for the surgery, which may include dietary modifications, physical activity recommendations, and pre-operative tests.
Immediately After Gastric Sleeve Surgery: After the surgery, you will spend a short period in the hospital for monitoring and recovery. During this time, you will receive pain management, and your healthcare team will closely monitor your progress. You will be started on a liquid diet initially, gradually progressing to soft and then solid foods, following specific guidelines provided by your healthcare provider.
Get a $1000 Off on Gastric Bypass Surgery Miami
3 Months After Gastric Sleeve Surgery: By the three-month mark, you can expect several positive changes and improvements in your health and lifestyle:
- Weight Loss: At this stage, you would have experienced significant weight loss. However, the extent of weight loss can vary among individuals. On average, most individuals can expect to lose around 30% to 40% of their excess body weight within the first three months after gastric sleeve surgery.
- Improved Health Conditions: Many individuals notice improvements in obesity-related health conditions such as type 2 diabetes, high blood pressure, and sleep apnea. Weight loss can help alleviate symptoms and reduce the need for medications for these conditions. However, it’s important to continue working closely with your healthcare provider to manage any ongoing medical concerns.
- Dietary Changes: By this stage, you would have transitioned through the post-operative diet phases and would be able to consume a wider variety of foods. However, portion sizes will still be significantly smaller, and it is essential to follow the dietary guidelines provided by your healthcare team. Focus on nutrient-dense foods, adequate protein intake, and stay hydrated.
- Increased Energy and Activity: Many individuals experience a boost in energy levels and increased mobility as they lose weight. Regular physical activity becomes more manageable, leading to improved fitness levels and overall well-being. Gradually incorporate exercise into your routine as advised by your healthcare provider.
- Psychological and Emotional Changes: Weight loss and lifestyle changes can have a positive impact on your psychological well-being. You may experience increased confidence, improved body image, and a sense of accomplishment. However, it is important to address any psychological or emotional challenges that may arise and seek support from healthcare professionals, if needed.
Remember that individual experiences may vary, and it’s important to maintain regular follow-up appointments with your healthcare provider to monitor your progress, address any concerns, and make necessary adjustments to your treatment plan. Long-term success after gastric sleeve surgery depends on adopting a healthy lifestyle, including a balanced diet, regular exercise, and ongoing support from your healthcare team.
Get a $1000 Off on Gastric Sleeve in Miami
Post-Operative Care and Recovery in the First 3 Months
After undergoing gastric sleeve surgery, proper post-operative care and recovery are crucial for achieving successful weight loss and maintaining overall health. Here are some important aspects of post-operative care during the first three months:
1. Hospital Stay and Immediate Recovery:
- Following surgery, you will spend a few days in the hospital for close monitoring and recovery.
- During this time, you will receive pain management, intravenous fluids, and be gradually introduced to a liquid diet.
- Your healthcare team will closely monitor your vital signs, incision sites, and overall progress.
2. Diet and Nutrition:
- Your diet will progress gradually to allow your stomach to heal and adjust to its new size.
- Initially, you will follow a liquid diet, consuming clear liquids and protein shakes.
- Over the next several weeks, you will transition to pureed and soft foods before gradually reintroducing solid foods.
- It’s important to follow your healthcare provider’s dietary guidelines and consume nutrient-rich foods to support healing and adequate nutrition.
3. Physical Activity and Exercise:
- Engaging in physical activity is important for maintaining muscle tone, improving circulation, and supporting weight loss.
- Follow your healthcare provider’s recommendations regarding when and how to start exercising.
- Initially, focus on light activities such as walking, gradually increasing intensity and duration as tolerated.
- Regular exercise can help enhance weight loss, improve cardiovascular health, and boost overall well-being.
4. Medications and Supplements:
- Your healthcare provider may prescribe medications to manage pain, prevent infection, and control acid reflux if needed.
- It is important to take medications as prescribed and report any adverse reactions or concerns to your healthcare provider.
- You may also need to take vitamin and mineral supplements to address potential nutrient deficiencies after surgery.
5. Lifestyle Modifications and Support:
- Adopting a healthy lifestyle is crucial for long-term success after gastric sleeve surgery.
- Make dietary and portion control adjustments as guided by your healthcare provider or a registered dietitian.
- Attend support group meetings or consider individual counseling to address any psychological or emotional challenges that may arise.
- Regularly communicate with your healthcare team, attend follow-up appointments, and seek their guidance for ongoing support and monitoring.
6. Monitoring Weight Loss and Health Progress:
- Keep track of your weight loss progress, but remember that individual results may vary.
- Your healthcare provider will monitor your weight, overall health, and progress during follow-up appointments.
- They will assess any changes in medical conditions, adjust medications if necessary, and provide ongoing guidance to support your weight loss goals.
Remember to follow your healthcare provider’s instructions, attend scheduled appointments, and report any unusual symptoms or concerns promptly.
Physical and Emotional Changes After 3 Months
After undergoing gastric sleeve surgery, significant physical and emotional changes can occur as a result of weight loss and lifestyle modifications. Here are some common changes that individuals may experience after three months:
| Physical and Emotional Changes After 3 Months |
|---|
| 1. Weight Loss and Body Transformation |
| 2. Improved Health and Reduction in Obesity-related Conditions |
| 3. Increased Energy and Physical Fitness |
| 4. Dietary Changes and Improved Eating Habits |
| 5. Psychological and Emotional Well-being |
| 6. Adjustments to Lifestyle and Social Interactions |
| 7. Continued Support and Follow-up Care |
Weight Loss Progress: What to Expect After 3 Months
After undergoing gastric sleeve surgery, weight loss progress can vary among individuals. However, it is common to experience significant weight loss within the first three months. Here’s what you can generally expect in terms of weight loss progress after three months:
| Weight Loss Progress After 3 Months |
|---|
| 1. Average Weight Loss: 20% to 40% of excess body weight |
| 2. Rapid Initial Weight Loss |
| 3. Steady Progress: 1-2 pounds per week |
| 4. Non-Linear Progress: Plateaus may occur |
| 5. Individual Variations |
Tips for Success in the First 3 Months Post-Surgery
The first three months after gastric sleeve surgery are critical for establishing healthy habits and maximizing weight loss. Here are some tips to promote success during this important period:
- Follow Post-Operative Guidelines: Adhere to the dietary and activity guidelines provided by your healthcare team. These guidelines are designed to support healing, promote weight loss, and prevent complications. Stick to the recommended diet phases, portion sizes, and recommended physical activity levels.
- Stay Hydrated: Drink an adequate amount of water throughout the day. Aim for at least 64 ounces (8 cups) of water daily, unless otherwise advised by your healthcare provider. Proper hydration supports digestion, helps prevent constipation, and aids in overall well-being.
- Eat Nutrient-Dense Foods: Focus on consuming nutrient-rich foods such as lean proteins, vegetables, fruits, and whole grains. These foods provide essential vitamins, minerals, and fiber while helping you stay satisfied. Limit or avoid processed foods, sugary snacks, and beverages.
- Portion Control: Be mindful of portion sizes, especially during meals. The reduced stomach size after surgery requires eating smaller meals more frequently. Use a smaller plate or bowl to visually manage portion sizes and prevent overeating.
- Chew Thoroughly and Eat Slowly: Take the time to chew your food thoroughly and eat slowly. This aids digestion, prevents discomfort, and allows you to recognize feelings of fullness. Put down utensils between bites and savor the flavors of each meal.
- Engage in Physical Activity: Gradually incorporate physical activity into your daily routine as recommended by your healthcare provider. Start with low-impact exercises such as walking, swimming, or cycling. Regular physical activity supports weight loss, improves cardiovascular health, and boosts overall well-being.
- Attend Support Groups or Counseling: Joining a support group or seeking individual counseling can provide valuable emotional support and help you navigate the challenges of the post-surgery period. Interacting with others who have undergone similar experiences can offer insights, encouragement, and motivation.
- Track Your Progress: Keep a record of your weight, measurements, and dietary habits. Monitoring your progress can provide a sense of accomplishment and help identify areas for improvement. Use a journal, mobile app, or other tracking tools to stay organized and accountable.
- Focus on Self-Care: Prioritize self-care activities that promote relaxation, stress reduction, and emotional well-being. This can include activities like meditation, deep breathing exercises, getting enough sleep, and engaging in hobbies or activities you enjoy.
- Communicate with Your Healthcare Team: Stay in close communication with your healthcare team, attending follow-up appointments as scheduled. They can provide guidance, address any concerns or questions you may have, and make adjustments to your treatment plan if needed.
Remember, the first three months post-surgery are an important period of adjustment and lifestyle transformation. By following these tips and maintaining a positive mindset, you can set a solid foundation for long-term success in your weight loss journey.

Importance of Support and Regular Medical Follow-ups
After undergoing gastric sleeve surgery, support and regular medical follow-ups play a crucial role in ensuring long-term success and optimal health. Here are key reasons why support and regular follow-ups are essential:
1. Emotional and Psychological Support:
- Support groups, counseling, or therapy can provide a safe space to discuss challenges, share experiences, and receive guidance.
- Emotional support is vital for coping with lifestyle changes, addressing body image concerns, and managing any psychological issues that may arise during the weight loss journey.
2. Nutritional Guidance:
- Registered dietitians or nutritionists can provide personalized dietary guidance, ensuring you meet your nutritional needs and maintain a balanced diet.
- Regular follow-ups allow for monitoring of dietary habits, assessing nutrient intake, and addressing any concerns related to nutrition.
3. Weight Loss Monitoring:
- Regular medical follow-ups enable healthcare providers to track your weight loss progress and adjust your treatment plan as needed.
- They can monitor changes in body composition, evaluate the effectiveness of interventions, and provide support and encouragement to help you stay on track.
4. Early Detection and Management of Complications:
- Regular follow-ups facilitate the early detection and management of any potential complications or side effects related to the surgery.
- Healthcare providers can assess your overall health, perform relevant tests, and address any concerns or symptoms that may arise.
5. Medication and Supplement Evaluation:
- Healthcare providers can review your medications and supplements to ensure they are appropriate for your current health status and weight loss journey.
- They can make adjustments, monitor potential interactions, and advise on the need for specific supplements to address any nutritional deficiencies.
6. Health Condition Management:
- Regular follow-ups allow healthcare providers to monitor and manage any pre-existing health conditions, such as diabetes or high blood pressure, as weight loss may impact medication dosages or treatment plans.
By actively participating in support groups, attending counseling sessions, and scheduling regular medical follow-ups, you can ensure that you receive comprehensive care, address any concerns promptly, and maintain a healthy and successful weight loss journey.
Dietary Changes in the First 3 Months After Gastric Sleeve Surgery
The first three months after gastric sleeve surgery are crucial for adjusting to your new stomach size and promoting successful weight loss. Here are the dietary changes that are typically necessary during this period:
| Dietary Changes in the First 3 Months After Gastric Sleeve Surgery |
|---|
| 1. Transitioning Diet Phases: Gradually progress from clear liquids to full liquids, pureed foods, and eventually solid foods, as recommended by your healthcare provider. Follow specific guidelines for each phase. |
| 2. Small, Frequent Meals: Consume smaller portion sizes and aim for three balanced meals per day. Include nutrient-dense foods such as lean protein, vegetables, fruits, and whole grains. Incorporate two to three healthy snacks between meals. |
| 3. Protein Intake: Ensure adequate protein intake to support healing and promote satiety. Consume protein-rich foods such as lean meats, poultry, fish, eggs, tofu, Greek yogurt, and legumes. Aim for a minimum of 60 to 80 grams of protein per day. |
| 4. Hydration: Stay hydrated by drinking at least 64 ounces (8 cups) of water daily, unless otherwise advised by your healthcare provider. Avoid carbonated beverages, caffeine, and sugary drinks. |
| 5. Avoidance of Problematic Foods: Steer clear of carbonated beverages, spicy foods, high-sugar foods and beverages, greasy or fried foods, and tough or fibrous meats, as they may cause discomfort or digestive issues. Observe how your body responds to different foods and make adjustments accordingly. |
| 6. Slow and Mindful Eating: Chew your food thoroughly and eat slowly to aid digestion and prevent discomfort. Take small bites, put down utensils between bites, and focus on savoring the flavors. Stop eating when you feel comfortably satisfied. |
| 7. Vitamin and Mineral Supplementation: Take prescribed vitamin and mineral supplements to prevent deficiencies. These may include multivitamins, calcium, vitamin D, iron, and vitamin B12. Follow the recommended dosage and schedule provided by your healthcare provider. |