A hiatal hernia is a condition where a portion of the stomach pushes through the diaphragm into the chest cavity. It can occur after gastric sleeve surgery, although it is relatively uncommon.
Get a $1000 Off on Gastric Sleeve in Miami
Incidence and Causes of Hiatal Hernia Post-Surgery
Hiatal hernia is a condition where a portion of the stomach protrudes through the diaphragm into the chest cavity. While hiatal hernias can occur after gastric sleeve surgery, they are relatively uncommon. Here is some information about the incidence and possible causes of hiatal hernia post-surgery:
Incidence: The exact incidence of hiatal hernia after gastric sleeve surgery is not well-defined. However, studies suggest that the occurrence of hiatal hernias following gastric sleeve surgery ranges from 1% to 10% of patients.
Possible Causes: Several factors can contribute to the development of hiatal hernia post-surgery:
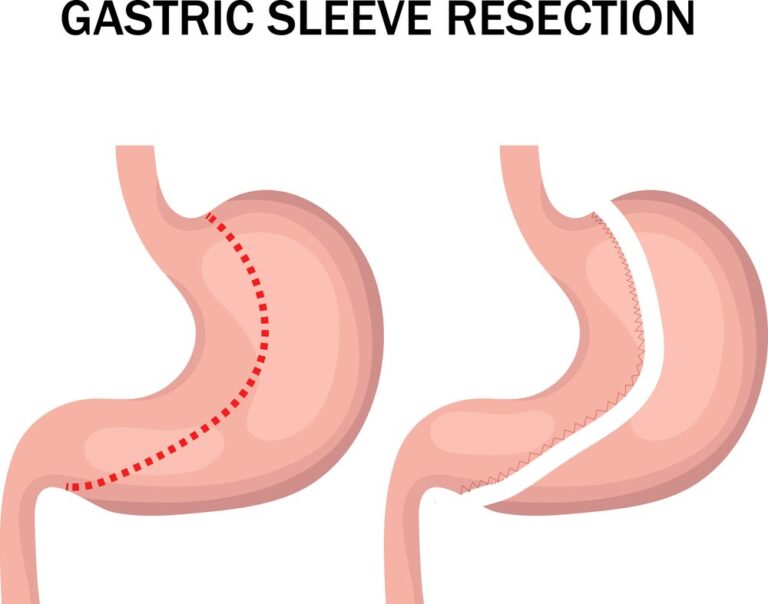
- Anatomical Changes: Gastric sleeve surgery involves removing a large portion of the stomach, which alters the anatomy of the stomach and surrounding structures. This can lead to changes in the position and function of the remaining stomach, potentially increasing the risk of a hiatal hernia.
- Weakness in the Diaphragm: The surgical procedure and subsequent weight loss can cause changes in the diaphragm, the muscle that separates the chest cavity from the abdomen. Weakened or disrupted diaphragmatic support may allow the stomach to push through the diaphragmatic opening, resulting in a hiatal hernia.
- Increased Intra-Abdominal Pressure: After gastric sleeve surgery, there can be an increase in intra-abdominal pressure due to changes in eating habits or post-surgical complications. This elevated pressure can contribute to the development of a hiatal hernia.
- Obesity and Pre-existing Hiatal Hernia: Obesity is a known risk factor for both hiatal hernias and gastric sleeve surgery. Individuals with pre-existing hiatal hernias or a higher BMI may be at increased risk of developing a hiatal hernia after gastric sleeve surgery.
Consult with Your Healthcare Provider: If you are experiencing symptoms or have concerns about a hiatal hernia after gastric sleeve surgery, it is important to consult with your healthcare provider. They can evaluate your condition, perform diagnostic tests if necessary, and recommend appropriate treatment options based on your individual circumstances.

Managing a hiatal hernia may involve lifestyle modifications, such as dietary changes and weight management. In some cases, surgical intervention may be necessary to repair the hernia. Your healthcare provider will guide you through the available options and develop a personalized treatment plan tailored to your needs.
How to fix hiatal hernia after gastric sleeve
If lifestyle modifications and medications do not effectively manage a hiatal hernia after gastric sleeve surgery, or if there are complications such as a large hernia or persistent symptoms, surgical intervention may be necessary. Here are some common surgical options to fix a hiatal hernia after gastric sleeve:
- 1. Hiatal Hernia Repair with Nissen Fundoplication: Nissen fundoplication is a surgical procedure commonly used to repair hiatal hernias. It involves repositioning the stomach to its normal position below the diaphragm and reinforcing the weakened diaphragmatic opening. The upper part of the stomach (fundus) is wrapped around the lower esophagus to create a valve, preventing acid reflux and reducing the risk of hernia recurrence.
- 2. Hiatal Hernia Repair with Mesh Reinforcement: In cases where the hiatal hernia is large or recurrent, the surgeon may use a mesh reinforcement technique during the repair. The mesh provides additional support to strengthen the diaphragmatic opening and reduce the chances of hernia recurrence.
- 3. Conversion to Gastric Bypass Surgery: In some situations, converting the gastric sleeve to a gastric bypass procedure may be recommended to address the hiatal hernia. Gastric bypass surgery involves rerouting the digestive system, bypassing a portion of the stomach and the upper small intestine. This can alleviate the symptoms of hiatal hernia by reducing acid reflux and repositioning the stomach below the diaphragm.
The choice of surgical option depends on the severity of the hiatal hernia, the presence of complications, and the individual’s overall health condition. It is essential to consult with a qualified bariatric surgeon to evaluate your specific situation and determine the most appropriate surgical approach.
During the consultation, the surgeon will discuss the risks, benefits, and expected outcomes of each procedure. They will consider factors such as the size of the hiatal hernia, the presence of other medical conditions, and your individual preferences to guide the decision-making process.
Symptoms and Diagnosis of Hiatal Hernia
Hiatal hernia is a condition where a portion of the stomach protrudes through the diaphragm into the chest cavity. It can cause a variety of symptoms, and diagnosing hiatal hernia typically involves a combination of clinical evaluation and diagnostic tests. Here is an overview of the symptoms and diagnosis of hiatal hernia:
| Symptoms of Hiatal Hernia |
|---|
| 1. Heartburn |
| 2. Acid Reflux |
| 3. Chest Pain |
| 4. Difficulty Swallowing |
| 5. Feeling Fullness or Bloating |
| 6. Shortness of Breath |
| Diagnosis of Hiatal Hernia |
|---|
| 1. Physical Examination |
| 2. Imaging Tests |
| 3. Endoscopy |
| 4. Esophageal Manometry |
Treatment and Prevention of Hiatal Hernia After Gastric Sleeve
Managing and preventing hiatal hernia after gastric sleeve surgery involves a combination of lifestyle modifications, medications, and, in some cases, surgical intervention. Here are some approaches to treat and prevent hiatal hernia:
1. Lifestyle Modifications:
- Dietary Changes: Avoiding trigger foods that can worsen symptoms, such as spicy or acidic foods, can help reduce acid reflux and discomfort. Eating smaller, more frequent meals and avoiding late-night eating can also alleviate symptoms.
- Weight Management: Maintaining a healthy weight through a balanced diet and regular exercise can help prevent excessive pressure on the abdomen, reducing the risk of hiatal hernia.
- Posture and Body Mechanics: Maintaining good posture during and after meals, such as sitting upright and avoiding slouching or lying down immediately after eating, can help prevent acid reflux and reduce symptoms.
2. Medications:
- Antacids: Over-the-counter antacids can help neutralize stomach acid and provide temporary relief from heartburn and acid reflux symptoms.
- Proton Pump Inhibitors (PPIs): These prescription medications reduce stomach acid production and can provide more long-term relief from acid reflux symptoms.
3. Surgical Intervention:
- Hernia Repair Surgery: In cases where lifestyle modifications and medications do not effectively manage the hiatal hernia, or if there are complications such as a large hernia or persistent symptoms, surgical repair may be necessary. This procedure typically involves returning the stomach to its normal position and reinforcing the diaphragm.
Prevention:
While it may not be possible to completely prevent hiatal hernia after gastric sleeve surgery, there are some measures that may help reduce the risk:
- Choose an Experienced Surgeon: Opt for a skilled and experienced surgeon who follows proper surgical techniques to minimize the risk of hiatal hernia during the gastric sleeve procedure.
- Follow Post-Operative Guidelines: Adhere to the post-operative guidelines provided by your healthcare team, including dietary recommendations, physical activity guidelines, and lifestyle modifications.
- Maintain a Healthy Weight: Focus on maintaining a healthy weight through a balanced diet and regular exercise to minimize the risk of abdominal pressure and hiatal hernia.
- Avoid Straining During Bowel Movements: Straining during bowel movements can increase abdominal pressure. Ensure adequate hydration, a fiber-rich diet, and consider stool softeners if needed to prevent straining.
It’s important to consult with your healthcare provider for personalized advice and treatment options based on your specific situation. They will assess your symptoms, evaluate the size and severity of the hiatal hernia, and recommend the most appropriate approach to manage and prevent further complications.

What is a Hiatal Hernia?
A hiatal hernia is a condition where a portion of the stomach pushes through the diaphragm into the chest cavity. The diaphragm is a muscular sheet that separates the chest cavity from the abdomen. It has an opening called the hiatus, through which the esophagus passes to connect to the stomach.
There are two main types of hiatal hernias:
- Sliding Hiatal Hernia: This is the most common type. In a sliding hiatal hernia, the junction where the esophagus meets the stomach and the top part of the stomach slide up into the chest through the hiatus. This can cause a portion of the stomach to be positioned above the diaphragm.
- Paraesophageal Hiatal Hernia: In this less common type, a part of the stomach squeezes through the hiatus and lies alongside the esophagus in the chest. The junction of the esophagus and stomach remains in its normal location below the diaphragm.
Potential Complications After Gastric Sleeve Surgery
While gastric sleeve surgery is generally safe and effective, like any surgical procedure, it carries some potential risks and complications. It is important to be aware of these potential complications and discuss them with your healthcare provider before undergoing surgery. Here are some of the possible complications associated with gastric sleeve surgery:
1. Surgical Complications:
- Infection: Infections can occur at the site of the incisions or within the abdominal cavity. They may require antibiotics or additional treatment.
- Bleeding: Excessive bleeding during or after surgery may require blood transfusion or surgical intervention to control bleeding.
- Leakage: A leak can occur along the staple line used to create the smaller stomach pouch. It may require surgical repair or additional interventions to address the leakage.
- Blood Clots: Blood clots, also known as deep vein thrombosis (DVT) or pulmonary embolism (PE), can form in the legs or travel to the lungs. Preventive measures, such as blood thinners and early ambulation, are usually taken to minimize this risk.
2. Digestive System Complications:
- Gastroesophageal Reflux Disease (GERD): Some individuals may experience worsened or new-onset GERD symptoms after gastric sleeve surgery. This can include heartburn, regurgitation, or difficulty swallowing.
- Stricture: Narrowing of the stomach opening or the connection between the stomach and small intestine (known as the pylorus) can occur, causing difficulties in food passage. Endoscopic dilation or revision surgery may be needed to alleviate the stricture.
3. Nutritional and Metabolic Complications:
- Malnutrition: Inadequate intake of essential nutrients, such as vitamins and minerals, can occur if dietary recommendations and supplementation guidelines are not followed. Regular monitoring and appropriate supplementation can help prevent malnutrition.
- Vitamin and Mineral Deficiencies: Gastric sleeve surgery can lead to decreased absorption of certain vitamins and minerals. Deficiencies in nutrients like vitamin B12, iron, calcium, and vitamin D may occur and require long-term supplementation.
4. Other Complications:
- Excess Weight Loss or Weight Regain: Some individuals may experience either excessive weight loss or weight regain following gastric sleeve surgery. Close monitoring and adherence to dietary and lifestyle recommendations can help optimize weight management.
- Psychological and Emotional Issues: Post-surgery, some individuals may experience psychological and emotional challenges, including body image concerns, depression, or disordered eating. Regular follow-up appointments and support from mental health professionals are essential.
It’s important to note that while these complications can occur, they are relatively rare. Most individuals undergo gastric sleeve surgery without experiencing significant complications.
Medical and Surgical Options for Hiatal Hernia Treatment
The treatment approach for hiatal hernias depends on the severity of symptoms, the size of the hernia, and the impact on an individual’s quality of life. Here are the medical and surgical options commonly used for hiatal hernia treatment:
1. Medical Management:
- Medications: Over-the-counter antacids can help neutralize stomach acid and provide temporary relief from heartburn and acid reflux symptoms. Proton pump inhibitors (PPIs) are prescription medications that reduce stomach acid production and can provide more long-term relief from acid reflux symptoms.
- Lifestyle Modifications: Making certain lifestyle changes can help manage hiatal hernia symptoms. These include avoiding trigger foods that worsen acid reflux (e.g., spicy or fatty foods), eating smaller meals, avoiding lying down immediately after eating, and maintaining a healthy weight.
2. Surgical Intervention:
- Hiatal Hernia Repair: Surgical repair is often recommended for hiatal hernias that cause significant symptoms or complications. The surgical procedure typically involves repositioning the stomach and repairing the weakened diaphragmatic opening. This can be done through open surgery or minimally invasive techniques such as laparoscopic surgery.
- Nissen Fundoplication: Nissen fundoplication is a surgical procedure used to treat hiatal hernias associated with severe gastroesophageal reflux disease (GERD). It involves wrapping the upper part of the stomach (fundus) around the lower esophagus to create a valve and prevent acid reflux.
- Hiatal Hernia Mesh Repair: In cases of larger or recurrent hiatal hernias, mesh reinforcement may be used during surgery to provide additional support and reduce the risk of hernia recurrence.
- Laparoscopic Gastric Bypass: In individuals with both obesity and hiatal hernia, laparoscopic gastric bypass surgery may be considered. This procedure involves rerouting the digestive system, bypassing a portion of the stomach and the upper small intestine. It can help address hiatal hernia symptoms and promote weight loss simultaneously.
The choice of treatment depends on various factors, including the size of the hernia, the severity of symptoms, the presence of complications, and individual patient characteristics. It is important to consult with a qualified healthcare provider or a bariatric surgeon to determine the most appropriate treatment option based on your specific situation.